IPF Patients Live Longer on Ofev Compared with Placebo, Analysis Suggests
Treatment with Ofev (nintedanib) can significantly extend the survival of patients with idiopathic pulmonary fibrosis (IPF), an analysis of pooled data from six clinical trials suggests.
The analysis, conducted by an international research team, was published in the journal BMJ Open Respiratory Research, in an article titled “Safety and survival data in patients with idiopathic pulmonary fibrosis treated with nintedanib: pooled data from six clinical trials.”
Ofev (marketed by Boehringer Ingelheim in the U.S., and as Vargatef in the E.U.) is an inhibitor of tyrosine kinases, which are important mediators of several growth factor signals known to be involved in IPF. The therapy was approved in October 2014 by the U.S. Food and Drug Administration, and in January 2015 by the European Medicines Agency for the treatment of IPF.
The decision to approve the therapy was supported by results of several controlled Phase 2 and 3 clinical trials. These included the Phase 2 TOMORROW trial (NCT00514683) and its open-label extension (NCT01170065), the two replicate Phase 3 INPULSIS trials (NCT01335464) and (NCT01335477) and their open-label extension INPULSIS-ON (NCT01619085), and also an exploratory Phase 3b study (NCT01979952).
These trials demonstrated that treatment with Ofev could significantly prevent disease progression by slowing the rate of decline in forced vital capacity — a measure of lung function — in patients with mild-to-moderate IPF.
None of the individual clinical trials were designed to evaluate the impact of the treatment on a patient’s survival time. However, mathematical models of the earlier data from the TOMORROW and INPULSIS studies had suggested that Ofev may reduce the risk of death by 30% compared with a placebo over 52 weeks of treatment.
To further explore Ofev’s effects on survival, an international research team conducted a new analysis of the pooled data from all six Ofev clinical trials. Pooling data is a mathematical technique that allows data from several different clinical trials to be analyzed together as if they were all from one trial. No new clinical trials were conducted that specifically examined Ofev’s effects on survival.
The analysis included data collected from 1,126 patients with IPF who were enrolled in any of the six prior clinical trials of Ofev and who received 150 mg twice daily during the trial. Data from 565 patients with IPF who received placebo when they were enrolled in the Phase 2 TOMORROW trial, the two replicate Phase 3 INPULSIS trials, or the exploratory Phase 3b study were also included.
The average age of the patients was 66.9 years in the Ofev 150 mg twice daily group and 66.6 years in the placebo group.
Participants received Ofev treatment for an average period of 27.7 months, with some patients receiving the treatment for a maximum of 93.1 months. In comparison, patients in the placebo group received a non-active compound for shorter periods of time, with a mean exposure of 10.4 months, up to a maximum of 13.1 months.
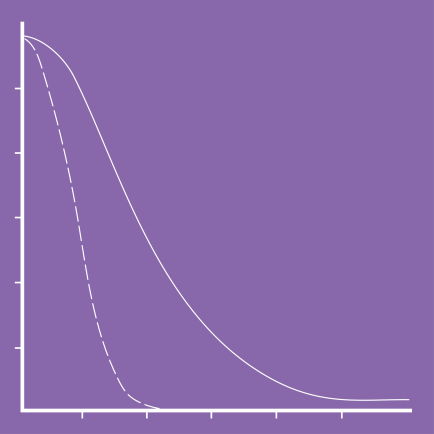
Using FVC results from the six clinical trials, the researchers were able to use mathematical models to estimate patients’ survival time. In the models, survival was found to be significantly longer with Ofev treatment than with placebo. Patients treated with Ofev had an estimated average survival time of 11.6 years from the start of treatment. Patients who received placebo had an estimated average survival time of 3.7 years from the start of receiving placebo. Therefore, the estimated survival time was approximately three times longer for patients treated with Ofev than for patients receiving placebo.
“Exploratory analyses based on extrapolation of survival data suggested that patients with IPF who are treated with nintedanib have longer life expectancy than those who do not receive treatment,” the researchers wrote.
Diarrhea was the most frequent side effect among patients treated with Ofev, with a higher incidence than in the pooled placebo group. Also, diarrhea was the most frequent side effect that led to permanent Ofev dose reduction or treatment discontinuation.
To manage the effects of diarrhea while taking Ofev, the team recommended that patients should “ensure adequate hydration and take antidiarrheal medicine.”
Other less common adverse events from Ofev treatment were increased liver enzyme levels, bleeding, major adverse cardiovascular events, and myocardial infarction (heart attack).
“Based on pooled data from six clinical trials, the adverse event profile of nintedanib was manageable for most patients,” the researchers wrote. They emphasized, however, that the medication should be taken by patients with a known risk of bleeding “only if the anticipated benefit outweighs the potential risk.”
Adapted from pulmonaryfibrosisnews.com